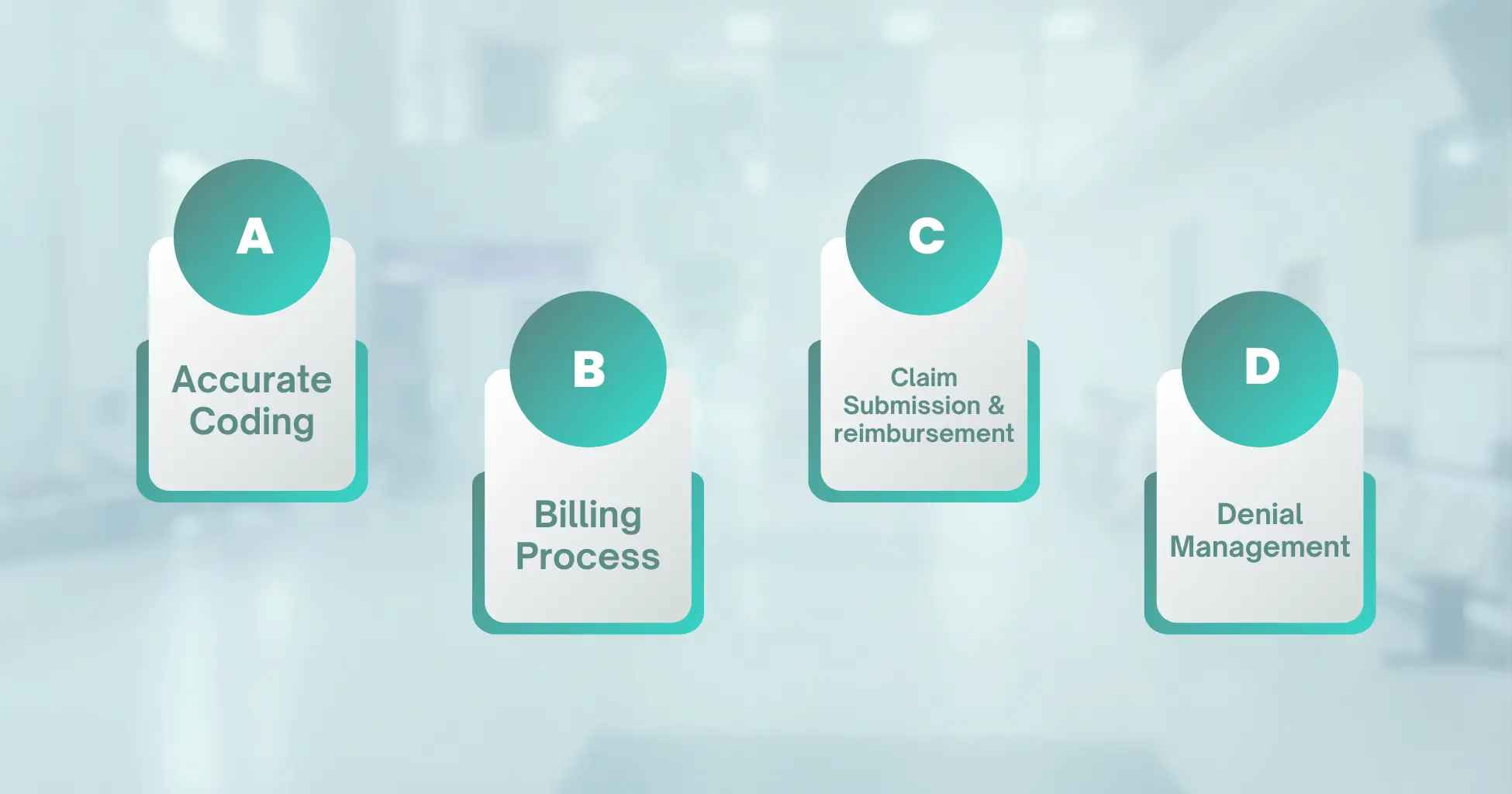
A - Accurate Coding
B - Billing Process
C - Claim Submission and Reimbursement
D - Denial Management
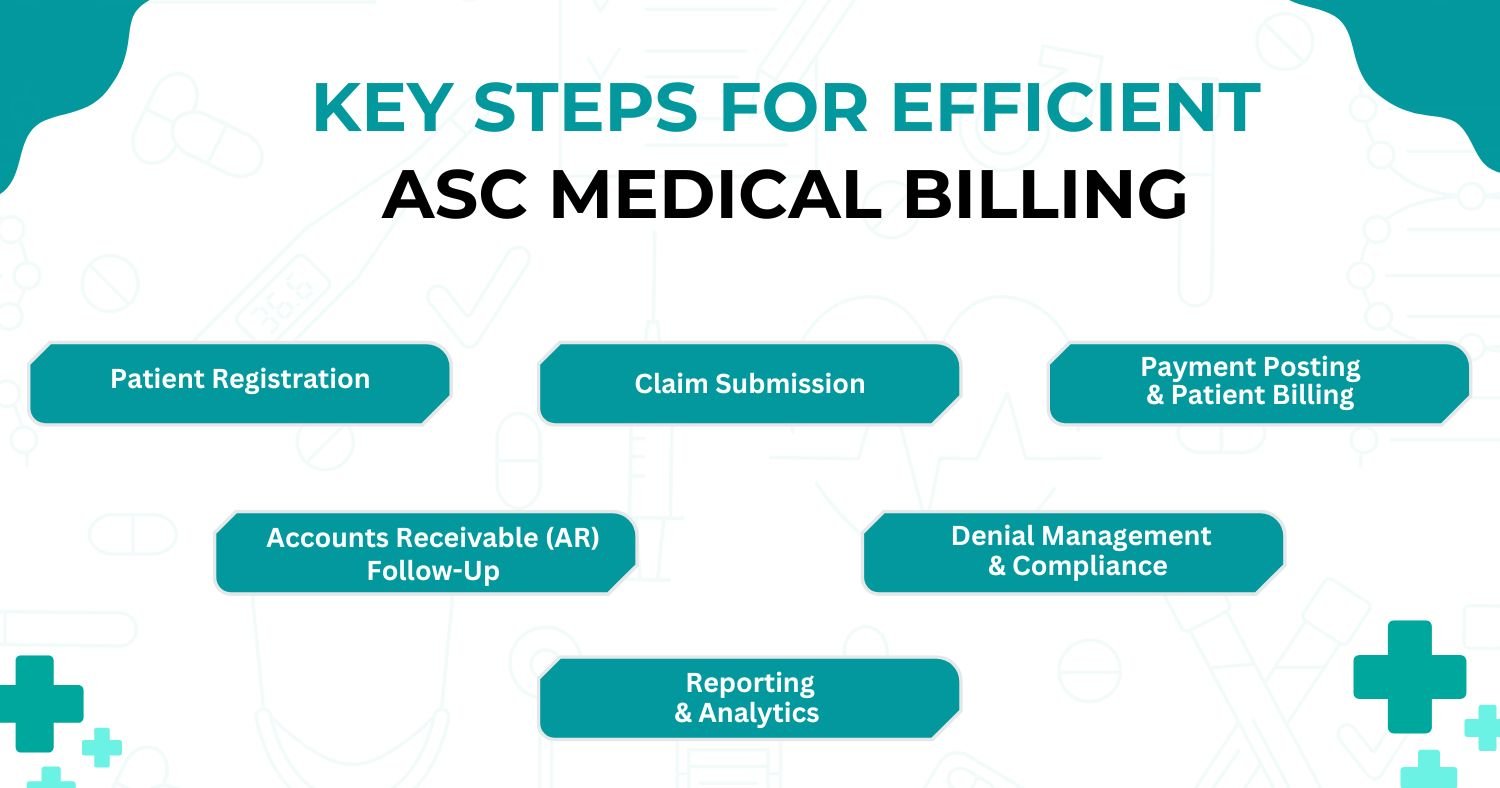
Denial management is an integral part of medical billing. Denials occur when insurance companies reject or refuse to reimburse a claim. It is crucial to have robust denial management processes in place to identify and resolve claim denials promptly. This involves analyzing denial reasons, correcting errors, providing additional documentation if required, and resubmitting claims. Effective denial management minimizes revenue loss and improves cash flow.
Accurate coding, proper billing processes, and timely claim submission are essential to optimize revenue cycle management and ensure prompt reimbursement. By adhering to standardized coding practices, following proper billing procedures, and staying updated with insurance guidelines, healthcare providers can streamline their billing operations and enhance financial efficiency. Moreover, continuous learning and keeping up with industry changes and regulatory requirements will contribute to successful medical billing practices.